This article is written by Ayushi Dubey, a third-year student of Institute of Law, Nirma University. The article highlights the concern towards the maternal health conditions of the country. The author has examined the current situation of maternal health conditions in the country and has pointed out the need towards their betterment. Through the article the author has raised two relevant questions and tried to answer them with respect to the ongoing condition of the country.
Introduction
Being able to give a new life is considered to be one of the greatest privileges. But great privilege comes with great responsibilities. A mother has to face a lot of issues during the course of her pregnancy, these issues could be economical or health-related as well. This article would be focusing on the health issues related to pregnancy and also what the state is doing for the same.
|
Selected State-wise Maternal Mortality Ratio (MMR), Maternal Mortality Rate and Life Time Risk in India (2014-2016) |
|||||||
|
States |
Sample Female Population |
Live Births |
Maternal Deaths |
Maternal Mortality Ratio |
95% CI |
Maternal Mortality Rate |
Lifetime Risk (%) |
|
Assam |
180780 |
12334 |
29 |
237 |
(151-323) |
16.2 |
0.6 |
|
Bihar/Jharkhand |
391838 |
37641 |
62 |
165 |
(124-206) |
15.8 |
0.6 |
|
Madhya Pradesh/Chhattisgarh |
409030 |
37106 |
64 |
173 |
(131-215) |
15.7 |
0.5 |
|
Odisha |
285319 |
19498 |
35 |
180 |
(121-240) |
12.3 |
0.4 |
|
Rajasthan |
249729 |
23082 |
46 |
199 |
(141-256) |
18.3 |
0.6 |
|
Uttar Pradesh/Uttarakhand |
621153 |
52843 |
106 |
201 |
(163-239) |
17.1 |
0.6 |
|
Empowered Action Group (EAG) and Assam |
2137849 |
182504 |
342 |
188 |
(168-207) |
16 |
0.6 |
|
Andhra Pradesh |
323541 |
15995 |
12 |
74 |
(32-116) |
3.6 |
0.1 |
|
Telangana |
208979 |
10840 |
9 |
81 |
(27-134) |
4.2 |
0.1 |
|
Karnataka |
299276 |
23341 |
25 |
108 |
(66-150) |
8.4 |
0.3 |
|
Kerala |
332361 |
15229 |
7 |
46 |
(12-79) |
2.1 |
0.1 |
|
Tamil Nadu |
285844 |
22552 |
15 |
66 |
(32-99) |
5.2 |
0.2 |
|
South |
1450001 |
87957 |
67 |
77 |
(58-95) |
4.7 |
0.2 |
|
Gujarat |
357416 |
25241 |
23 |
91 |
(54-129) |
6.4 |
0.2 |
|
Haryana |
182102 |
14707 |
15 |
101 |
(50-152) |
8.2 |
0.3 |
|
Maharashtra |
384107 |
23172 |
14 |
61 |
(29-93) |
3.7 |
0.1 |
|
Punjab |
160608 |
9097 |
11 |
122 |
(50-194) |
6.9 |
0.2 |
|
West Bengal |
448410 |
24318 |
25 |
101 |
(61-141) |
5.5 |
0.2 |
|
Other States |
1175608 |
59865 |
58 |
97 |
(72-122) |
5 |
0.2 |
|
Other |
2708251 |
156400 |
146 |
93 |
(78-109) |
5.4 |
0.2 |
|
India |
6296101 |
426861 |
556 |
130 |
(119-141) |
8.8 |
0.3 |
|
Source: indiastat.com, https://www.indiastat.com. |
|||||||
The given data shows maternal deaths, maternal mortality ratio and risk involved of the year 2014-2016. The data clearly depicts that the risk involved is the least in the south Indian states, on top is Kerala, one of the reasons behind the same can be higher literacy rates in the state. The highest risk is found in the state of Assam and Bihar/Jharkhand i.e. 0.6, the major reasons behind this is again low literacy rates and large populations as well.
India has registered a 77 percent decline in the Maternal Mortality Ratio (MMR) from 556 per 100,000 live births in 1990 to 130 per 100,000 live births in 2016 [1]. The credit goes to a number of initiatives taken by the government. a large portion of victory is taken by the Janani Suraksha Yojana which has contributed to a surge in institutional deliveries from 38.7 per cent in 2005-06 to 78.9 percent in 2015-16 [2]. Other schemes such as Pradhan Mantri Surakshit Matratav Abhiyan in which private doctors voluntarily visit government hospitals on every 9th day of the month. A number of other policies will also be discussed in the article . Other than these policies indirect factors such as an increase in literacy rates and awareness towards health and hygiene also plays a crucial role in reducing maternal health-related issues. Research has also shown that the decline in poverty ratios and growth in per capita net state domestic product are major reasons for better maternal health conditions.
Two Important Questions
- Whether the policies and steps taken by the government of India for maternal health are enough?
- What India has done for maternal health as compared to other countries?
1.Whether the policies and steps taken by the Government of India for Maternal Health are enough?
This question would be discussed in different segments such as what all policies India has adopted, the current policies and the policies of the past which have been made dysfunctional now, the reasoning behind adopting the current policies and the problems in those policies and whether or not these policies have created any significant changes in the poor maternal health conditions of India.
1. Laqshya Standard Operating Procedures For District Hospitals [3]
Launched in November 2017 the said policy focuses on intrapartum and postpartum care as it is estimated that almost 46% of maternal deaths take place on the day of delivery. The primary objective of this initiative is to curb maternal mortality and morbidity, neonatal mortality and stillbirths. The policy majorly focuses on labour rooms and maternity operation theatres in district hospitals. The purpose is to create better conditions for pregnant women in hospitals by assisting health personnel in providing safe and hygienic conditions to women at district hospitals. The statement of purpose of the policy explains what steps should be followed by the health personnel in labour rooms, operation theatre and Central Sterile Supply Department. The large focus of the policy is on clinical procedures.

2. Janani Suraksha Yojana [4]
The scheme was launched in April 2005 in all states and union territories and with special focus on low performing states. The scheme is sponsored by the central government and provides cash assistance with delivery and post-delivery care. The main objective of the scheme is to promote institutional delivery so as to curb maternal and neonatal mortality among the poor pregnant women of society.
The eligibility for cash assistance under the JSY is as shown below[5]:
|
LPS |
All pregnant women delivering in government health centres, such as sub-centres (SCs)/Primary Health Centers (PHCs)/Community Health Centers (CHCs)/First Referral Units (FRUs)/general wards of district or state hospitals |
||||||
|
HPS |
All BPL/Scheduled Caste/Scheduled Tribe (SC/ST) women delivering in a government health centre, such as SC/PHC/CHC/FRU/general wards of district or state hospital |
||||||
|
LPS & HPS |
BPL/SC/ST women in accredited private institutions |
||||||
|
States/UTs |
Allocation of funds( in crores) |
||||||
|
2010- 2011 |
2011- 2012 |
2012- 2013 |
2013- 2014 |
2014- 2015 |
2015- 2016 |
2016-2017 (P) |
|
|
Andaman and Nicobar Islands |
0.12 |
0.06 |
0.11 |
0.06 |
0.07 |
0.07 |
0.07 |
|
Andhra Pradesh |
50.36 |
32.88 |
31.79 |
45.47 |
25.10 |
24.95 |
27.66 |
|
Arunachal Pradesh |
1.64 |
1.41 |
1.42 |
– |
1.82 |
2.31 |
2.02 |
|
Assam |
101.50 |
93.39 |
81.07 |
92.45 |
104.94 |
85.34 |
71.56 |
|
Bihar |
249.97 |
250.90 |
244.29 |
354.35 |
387.15 |
312.98 |
343.40 |
|
Chandigarh |
0.08 |
0.08 |
0.08 |
0.05 |
0.06 |
0.14 |
0.10 |
|
Chhattisgarh |
74.67 |
68.85 |
61.32 |
70.88 |
60.07 |
60.94 |
69.14 |
|
Dadra and Nagar Haveli |
0.14 |
0.15 |
0.13 |
0.14 |
0.22 |
0.22 |
0.53 |
|
Daman and Diu |
0.00 |
0.00 |
0.06 |
0.04 |
0.03 |
0.03 |
0.03 |
|
Delhi |
2.40 |
2.18 |
1.85 |
2.24 |
2.30 |
2.01 |
1.61 |
|
Goa |
0.10 |
0.10 |
0.12 |
0.12 |
0.12 |
0.12 |
0.12 |
|
Gujarat |
22.38 |
21.00 |
25.81 |
35.02 |
35.80 |
36.16 |
28.23 |
|
Haryana |
6.99 |
6.60 |
6.30 |
5.92 |
4.33 |
5.35 |
5.47 |
|
Himachal Pradesh |
2.18 |
1.90 |
2.33 |
2.11 |
2.27 |
3.10 |
2.66 |
|
Jammu and Kashmir |
20.80 |
21.93 |
20.57 |
22.40 |
28.12 |
30.88 |
24.32 |
|
Jharkhand |
70.22 |
69.70 |
89.25 |
89.71 |
86.41 |
94.72 |
71.43 |
|
Karnataka |
46.03 |
38.54 |
42.45 |
66.20 |
65.85 |
66.23 |
78.81 |
|
Kerala |
9.66 |
13.55 |
12.13 |
16.08 |
12.13 |
13.70 |
14.99 |
|
Lakshadweep |
0.05 |
0.07 |
0.06 |
0.08 |
0.07 |
0.12 |
0.12 |
|
Madhya Pradesh |
200.78 |
188.10 |
191.41 |
210.25 |
189.80 |
185.66 |
192.40 |
|
Maharashtra |
22.59 |
35.28 |
30.23 |
44.82 |
52.64 |
49.82 |
50.87 |
|
Manipur |
1.32 |
2.20 |
1.68 |
2.17 |
1.97 |
2.34 |
2.34 |
|
Meghalaya |
2.28 |
1.28 |
2.14 |
3.79 |
3.68 |
4.16 |
4.62 |
|
Mizoram |
1.64 |
1.78 |
1.39 |
1.70 |
1.88 |
1.29 |
1.29 |
|
Nagaland |
4.44 |
2.73 |
1.82 |
2.06 |
1.76 |
1.84 |
1.82 |
|
Odisha |
126.54 |
108.30 |
110.24 |
120.06 |
98.28 |
102.19 |
95.46 |
|
Puducherry |
0.33 |
0.34 |
0.35 |
0.35 |
0.30 |
0.27 |
0.27 |
|
Punjab |
6.12 |
6.46 |
8.07 |
10.43 |
11.09 |
11.09 |
10.82 |
|
Rajasthan |
143.68 |
184.10 |
181.41 |
217.11 |
194.08 |
201.00 |
176.29 |
|
Sikkim |
0.53 |
0.59 |
0.44 |
0.51 |
0.31 |
0.23 |
0.32 |
|
Tamil Nadu |
35.30 |
34.52 |
35.72 |
36.02 |
52.44 |
39.92 |
41.34 |
|
Telangana |
– |
– |
– |
– |
22.83 |
18.28 |
21.33 |
|
Tripura |
3.17 |
3.36 |
2.82 |
3.13 |
2.92 |
3.19 |
3.19 |
|
Uttar Pradesh |
400.01 |
475.30 |
521.90 |
471.24 |
509.21 |
511.85 |
511.29 |
|
Uttarakhand |
20.31 |
15.12 |
13.51 |
15.39 |
19.07 |
21.13 |
17.41 |
|
West Bengal |
54.18 |
58.37 |
60.16 |
74.44 |
59.67 |
69.76 |
56.40 |
|
India |
1682.48 |
1741.00 |
1809.67 |
2018.97 |
2039.81 |
1963.38 |
1929.75 |
Source: indiastat, https://www.indiastat.com
3. Janani Shishu Suraksha Karyakram [6]
Launched on 1st June 2011, is a scheme that covers both pregnant women and newborn child till 30 days of birth. The scheme provides the following facilities:
- Free and zero expense treatment.
- Free drugs and consumables.
- Free diagnostics & Diet.
- Free provision of blood.
- Free transport from home to health institutions.
- Free transport between facilities in case of referral.
- Drop back from institutions to home.
- Exemption from all kinds of user charges.
The scheme covers almost all issues related to maternal as well as newborn health. It provides easy accessibility to hospitals by cutting out transport and medical expenses.
|
State-wise Expenditure under Janani Shishu Suraksha Karyakaram (JSSK) in India (2011-2012 to 2016-2017) |
|||||||
|
(Rs. in Crore) |
|||||||
|
States/UTs |
2011-2012 |
2012-2013 |
2013-2014 |
2014-2015 |
2015-2016 |
2016-2017 |
|
|
Andaman and Nicobar Islands |
0.00 |
0.11 |
0.06 |
0.40 |
0.00 |
0.02 |
|
|
Andhra Pradesh |
0.00 |
31.79 |
45.47 |
22.48 |
28.72 |
60.17 |
|
|
Arunachal Pradesh |
0.00 |
1.42 |
2.18 |
1.38 |
1.94 |
1.38 |
|
|
Assam |
0.00 |
81.07 |
92.45 |
46.37 |
89.65 |
70.43 |
|
|
Bihar |
0.00 |
244.29 |
354.35 |
62.77 |
81.14 |
58.49 |
|
|
Chandigarh |
0.00 |
0.08 |
0.05 |
0.00 |
1.37 |
1.42 |
|
|
Chhattisgarh |
0.00 |
61.32 |
70.88 |
11.15 |
13.33 |
9.59 |
|
|
Dadra and Nagar Haveli |
0.00 |
0.13 |
0.14 |
0.25 |
0.39 |
0.96 |
|
|
Daman and Diu |
0.00 |
0.06 |
0.04 |
0.14 |
0.02 |
0.01 |
|
|
Delhi |
0.00 |
1.85 |
2.24 |
2.44 |
1.45 |
1.48 |
|
|
Goa |
0.00 |
0.12 |
0.12 |
0.82 |
0.28 |
0.56 |
|
|
Gujarat |
0.00 |
25.81 |
33.83 |
32.59 |
39.47 |
54.81 |
|
|
Haryana |
0.48 |
6.30 |
5.92 |
21.00 |
14.24 |
14.97 |
|
|
Himachal Pradesh |
2.50 |
2.33 |
2.11 |
16.60 |
20.51 |
17.91 |
|
|
Jammu and Kashmir |
0.56 |
20.57 |
22.40 |
23.59 |
30.65 |
34.51 |
|
|
Jharkhand |
0.00 |
89.25 |
89.71 |
44.03 |
44.21 |
51.52 |
|
|
Karnataka |
0.00 |
42.45 |
66.20 |
28.51 |
36.99 |
47.31 |
|
|
Kerala |
0.00 |
12.13 |
16.08 |
22.92 |
20.70 |
15.93 |
|
|
Lakshadweep |
0.00 |
0.06 |
0.08 |
0.12 |
0.05 |
0.04 |
|
|
Madhya Pradesh |
0.00 |
191.41 |
210.25 |
93.66 |
112.51 |
118.70 |
|
|
Maharashtra |
0.00 |
30.23 |
31.23 |
98.04 |
76.44 |
64.73 |
|
|
Manipur |
0.00 |
1.68 |
2.17 |
4.48 |
6.12 |
3.72 |
|
|
Meghalaya |
0.00 |
2.14 |
2.63 |
2.66 |
7.57 |
9.54 |
|
|
Mizoram |
0.00 |
1.39 |
1.39 |
0.87 |
0.55 |
0.67 |
|
|
Nagaland |
0.00 |
1.82 |
2.06 |
1.37 |
1.03 |
0.76 |
|
|
Odisha |
0.00 |
110.24 |
120.06 |
18.38 |
31.40 |
41.29 |
|
|
Puducherry |
0.00 |
0.35 |
0.35 |
2.36 |
0.98 |
2.96 |
|
|
Punjab |
0.00 |
8.07 |
10.43 |
26.14 |
27.83 |
38.47 |
|
|
Rajasthan |
7.69 |
181.41 |
217.11 |
118.11 |
90.90 |
110.02 |
|
|
Sikkim |
0.00 |
0.44 |
0.51 |
1.09 |
0.93 |
0.77 |
|
|
Tamil Nadu |
0.00 |
35.72 |
36.02 |
117.21 |
67.66 |
76.47 |
|
|
Telangana |
– |
– |
– |
19.40 |
18.26 |
26.38 |
|
|
Tripura |
0.86 |
2.82 |
3.13 |
4.36 |
4.92 |
6.67 |
|
|
Uttar Pradesh |
0.00 |
521.90 |
471.24 |
132.94 |
146.97 |
181.95 |
|
|
Uttarakhand |
0.00 |
13.51 |
15.39 |
16.84 |
21.30 |
16.42 |
|
|
West Bengal |
1.05 |
60.16 |
51.70 |
141.34 |
151.13 |
165.73 |
|
|
India |
13.14 |
1784.45 |
1979.98 |
1136.83 |
1191.58 |
1306.74 |
|
|
Source: Indiastat, https://www.indiastat.com |
|||||||
The table shows the fund that has been allocated by the government under the Janani Shishu Suraksha Karyakram for various states between 2011 and 2017.
4. Navjat Shishu Suraksha Karyakram [7] (Nssk)
The program focuses on “care at birth issues” i.e. Prevention of Hypothermia, Prevention of Infection, Early initiation of Breastfeeding and Basic Newborn Resuscitation. The main objective of the scheme is to develop a country where each delivery point has trained personnel in basic newborn care. The 2-day training is given to the personals with the expectation of reducing neonatal mortality significantly in the country.
5. Infant and young child feeding [8]
Focusing on child survival, this is the only intervention for the same in the country. The scheme has the following features:-
- Early initiation (within one hour of birth) and exclusive breastfeeding until 6 months.
- Timely complementary feeding after 6 months with continued breastfeeding till the age of 2 yrs.
There are a number of other policies also which work for improving maternal health conditions. Such as Pradhan Mantri Surakshit Matratav Abhiyan, Sakhi Centers, maternity benefit bill etc.
2. What India Has Done For Maternal Health As Compared To Other Countries?
The findings of the World Health Organization reveal that 45,000 Indian woman dies from preventable pregnancy-related complications in India [9]. The WHO also estimates that out of 5,36,000 maternal death occurring annually, 1,36,000 deaths occur in India itself, which constitutes 25% of the total maternal deaths in the world.[10] While India continued to focus upon Economic Development during the 1990s, it completely ignored the maternal health and nutrition health of the country which resulted in an increase in Under 5-years mortality rate, increased infant mortality rate, increase in maternal mortality rate and a decline in other health indicators as well.
Talking about South-Asian countries, India has acquired and continues to acquire a substantial position in South-Asian economy. It is because of the deteriorating maternal healthcare in the world, especially in the developing countries, the WHO has sought to achieve the fourth and fifth Millennium Development Goals (MDGs) of improved child survival and health. South Asia accounts for 20% of the population of the world that is why proper attention needs to be paid to the South-Asian countries. Thus, a comparative analysis of maternal and child healthcare of India with other developing South-Asian countries like Bangladesh, Sri-Lanka and Nepal would show that up to what extent the policies and programmes of India have been successful in achieving the Millennium Development Goals and improving Maternal and Child healthcare in India.
As discussed earlier, the major indicators of Maternal and Child Health and Nutrition, as depicted in the Millennium Development Goals, include Under-5 years Mortality Rate, Maternal Mortality Rate and Infant Mortality Rate. A comparative analysis of India with Sri-Lanka, Nepal and Bangladesh with respect to Under-5 years Mortality Rate shows that a decline has been there in all the four countries. Statistically, in the year 2000, India had the highest rate at 87.7 followed by Bangladesh at 84.4 and Nepal at 82.9. Sri-Lanka continues to have a low rate of Under-5 years of Mortality since the beginning [11]. A comparative statistical study of all the four countries with respect to Under-5 years Mortality Rate is depicted in the following Figure 1:
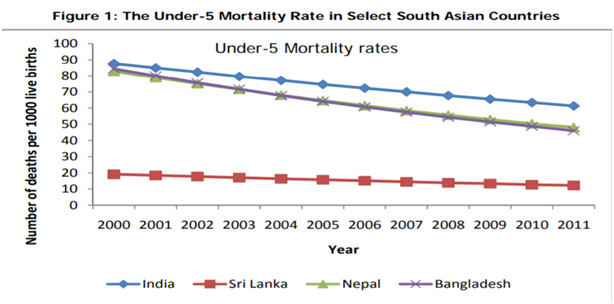
Source: http://mdgs.un.org/unsd/mdg/Data.aspx
The findings are similar as in the case of Infant Mortality Rate as well, which are depicted in Figure 2 which is as follows:
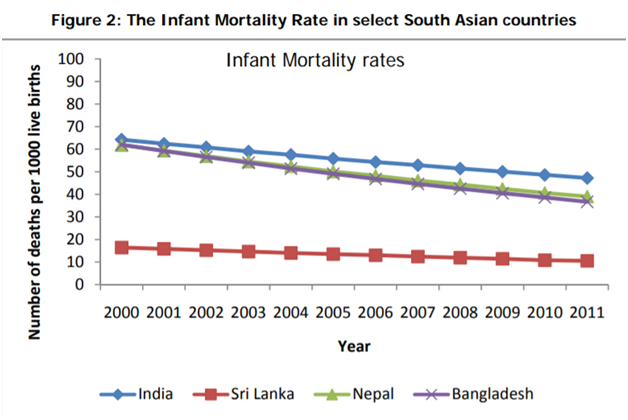
Source: http://mdgs.un.org/unsd/mdg/Data.aspx
Statistical analysis of Maternal Mortality Rate as depicted in Figure 3 which, reveals that there has been a declining trend in the Maternal Mortality Rate. Nepal has been an attention seeker in the present case, surpassing India and reducing its Maternal Mortality Rate. Bangladesh is close to India while Sri-Lanka still maintains low levels of Maternal Mortality Rate which is less than 100 deaths/1000 live births.[12]
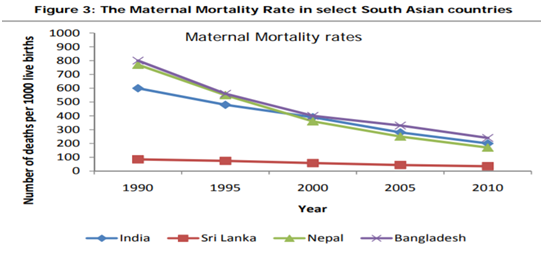
Source: http://mdgs.un.org/unsd/mdg/Data.aspx
All of the above statistics reveal that while India may have opted for various policies and programmes for effective implementation of improving Maternal and Child Healthcare, there has been no significant improvement in the abovementioned. The reason for the same is observed to be lack of proper governance, thereby resulting in an inefficient delivery system and deteriorating maternal as well as child health. Despite major programmes like National Rural Health Mission, which aims at expanding access to emergency obstetric and new-born care has increased the utilization with a positive effect on outcomes,[13] and Integrated Child Development Services being brought forward and launched by the Government of India, no significant improvement has been witnessed. India has also been receiving funds from the WHO and other international donors in the name of healthcare but the same has been utilized in other politically motivated areas. The above statistics clearly show that other South-Asian Developing countries have surpassed India in the matters of Maternal Health and Child healthcare.
Conclusion
The author has collected data from various reliable sources and has done intensive doctrinal and empirical research and have concluded that India still has a long way to go to achieve its goal so if the question is “whether India has done enough for maternal health” the answer would still be no, there is a long way to go, a number of policies have been formed but the policies lack in proper implementation. Poverty and illiteracy also contribute equally to poor maternal health conditions and high maternal mortality rates. Each country has different backgrounds and different economic conditions therefore, we can’t compare the policies of one country with another country. But, there are certain policies or scheme, if studied well, can have a global implementation. Hence, the author believes that India still has a lot to do in order to achieve good maternal health conditions, situations where a life is never sacrificed because of the lack of facilities and financial assistance. Hygienic and good health services are a basic right and should be given to all irrespective of their status. A woman suffers a lot and goes through a lot of problems during her pregnancy therefore, the state should take initiatives to improve living conditions for the to-be mother. Good health facilities will also affect the life of the newborn for the good. A healthy child would only act as an asset to the world.
References
[3]http://www.nhm.gov.in/nrhm-components/rmnch-a/child-health-immunization/child-health/guidelines.html
[4]http://www.nhm.gov.in/nrhm-components/rmnch-a/child-health-immunization/child-health/schemes.html
[5]http://nhm.gov.in/nrhm-components/rmnch-a/maternal-health/janani-suraksha-yojana/background.html
[6]http://www.nhm.gov.in/nrhm-components/rmnch-a/child-health-immunization/child-health/schemes.html
[7]http://www.nhm.gov.in/nrhm-components/rmnch-a/child-health-immunization/child-health/schemes.html
[8]http://www.nhm.gov.in/nrhm-components/rmnch-a/child-health-immunization/child-health/schemes.html
[9]file:///C:/Users/g/Downloads/maternal-health-mortality%20Source%201.pdf
[10]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2761784/
[11]http://www.isec.ac.in/WP%20323%20-%20K%20Gayithri_1.pdf
[12]http://www.isec.ac.in/WP%20323%20-%20K%20Gayithri_1.pdf
[13]https://ijmedph.org/sites/default/files/IntJMedPublicHealth_2014_4_1_33_127120.pdf,
 Serato DJ Crack 2025Serato DJ PRO Crack
Serato DJ Crack 2025Serato DJ PRO Crack









 Allow notifications
Allow notifications


